5 Strategies to Build a Care Coordination System that Works
Healthcare is very involved. Especially if a patient is very ill or has a chronic condition, there are likely many people involved in their care...
2 min read
 Lynn Corbitt
:
November 3, 2022
Lynn Corbitt
:
November 3, 2022
Healthcare providers need to be excellent at remembering how important their patients are and how much they rely on the providers to guide them through the healthcare process. Unless a patient works in healthcare, they likely don’t really know what’s going on, especially if they’re encountering a more major medical issue. They’re trying to navigate the health side of the experience and also the business and payments side, and it can all become stressful and overwhelming. Luckily, good providers are able to walk with their patients.
Many times a patient needs to be seen by more than one provider. When transfers happen, it’s important to make them as easy on the patient as possible. One way to do this is by establishing strong continuity of care. While it’s certainly easier to transfer a patient within a single healthcare system, sometimes that can’t happen. No matter what the transfer looks like, though, a continuity of care document can make the process easier.
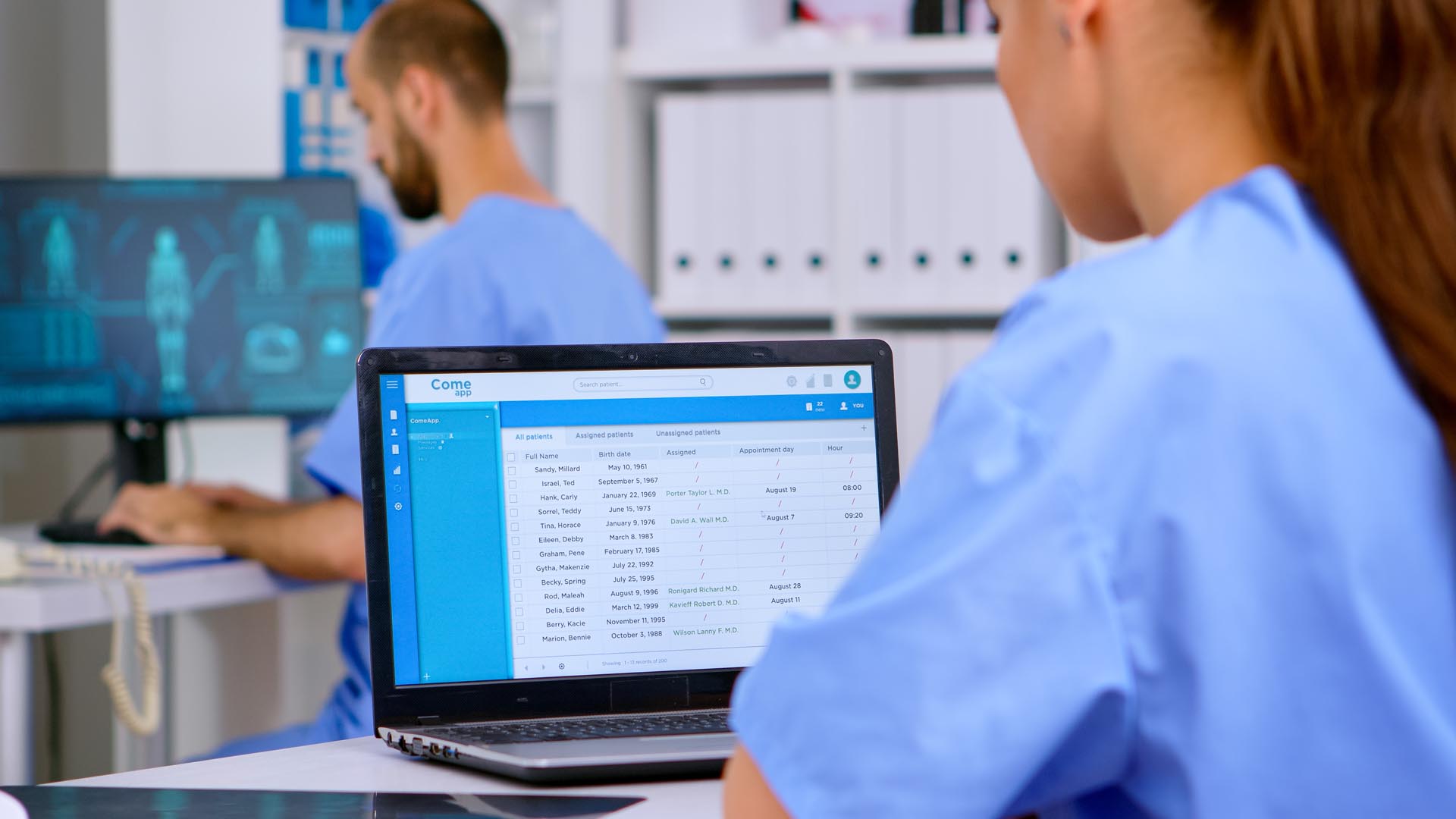
A continuity of care document is a very generic term for the report generated by an Electronic Health Record (EHR). It helps provide improved communication between the providers involved in the transfer, leading to a smoother transition and better patient experience. They include care summary information, as well as some basic patient history for the provider’s knowledge.
The CCD is what we’ve been talking about: a continuity of care document. Historically, this has been a paper document, so think of it as a printed version of an EHR summary.
A CDA is a document written in the “clinical document architecture.” This is totally electronic and is not printed. It also has to follow a certain style guide and contain very specific information.
The C-CDA stands for Consolidated Clinical Document Architecture, and is a guide for how to write a CDA so they can be easily exchanged throughout healthcare systems.
As you can see, all three of these are very similar. At the end of the day, healthcare providers and their system staff (hospitals, clinics, rehab centers, etc.) know what specific rules and guidelines they need to follow for compliance. The most important thing to a patient is that their providers are all on the same page and have the background they need to care for them properly.
EHRs are very important to accurately capturing patient data and storing it for future interpretation and analysis. When a patient is at a hospital, for example, nurses can log all of the patient’s data in their EHR, and the physicians can check and see if there have been any meaningful changes. However, when a patient is transferred from one hospital to somewhere else, outside of that hospital’s healthcare system, EHRs can’t simply be handed over on a thumb drive.
For patient safety and security, the data must be handed over securely, via the CCD we’ve been talking about. Some systems send all of the information, which can be overwhelming. Others send the bare minimum, and the new providers can be trying to fill in the gaps. The guidelines set by the C-CDA are designed to help alleviate these problems, but it’s still not a perfect outline, and it is often updated.
EHRs and CCDs allow providers to get to know their patients before they even look them in the eye. This background, baseline knowledge can help them provide more efficient, timely care, and it can help them move more quickly to the important part of their visit.
However, it’s important for providers to remember that patients are more than just the numbers and data and clinical notes on a CCD. They’re real people who are experiencing something that might be overwhelming. Technology is excellent, because it provides a chance to save time and have information transferred accurately. But it can mean a lot to patients for a provider to ask them in-depth, personal questions, rather than just assuming they know everything since they've read their file.

Healthcare is very involved. Especially if a patient is very ill or has a chronic condition, there are likely many people involved in their care...

A patient care coordinator works diligently to ensure patients receive the best possible care throughout their healthcare experience. Care...

When it comes to implementing an entertainment system at a long-term care facility, the signal source, head-end equipment, and installation process...